Pneumocystis jirovecii is a yeast-like fungus of the genus Pneumocystis. The causative organism of Pneumocystis pneumonia, it is an important human pathogen, particularly among immunocompromised hosts. Prior to its discovery as a human-specific pathogen, P. jirovecii was known as P. carinii.
Lifecycle

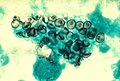
The complete lifecycles of any of the species of Pneumocystis are not known, but presumably all resemble the others in the genus. The terminology follows zoological terms, rather than mycological terms, reflecting the initial misdetermination as a protozoan parasite. It is an extracellular parasite. All stages are found in lungs and because they cannot be cultured ex vivo, direct observation of living Pneumocystis is difficult. The trophozoite stage is thought to be equivalent to the so-called vegetative state of other species (such as Schizosaccharomyces pombe) which, like Pneumocystis belong to the Taphrinomycotina branch of the fungal kingdom. The trophozoite stage is single-celled and appears amoeboid (multilobed) and closely associated with host cells. Globular cysts eventually form that have a thicker wall. Within these ascus-like cysts, eight spores form which are released through rupture of the cyst wall. The cysts often collapse forming crescent-shaped bodies visible in stained tissue. It is not known for certain if meiosis takes place within the cysts, or what the genetic status is of the various cell types.
Medical relevance
Pneumocystis pneumonia is an important disease of immunocompromised humans, particularly patients with HIV, but also patients with an immune system that is severely suppressed for other reasons; for example, following a bone marrow transplant. In humans with a normal immune system, it is an extremely common silent infection.
Identified by methenamine silver stain of lung tissue. Kills type 1 pneumocytes which decrease surfactant and causes death by asphyxiation. Drug of choice is TMP-SMX, pentamidine, or dapsone, make sure to check CD4 Tcell drop below 200.
Nomenclature

At first, the name Pneumocystis carinii was applied to the organisms found in both rats and humans, as it was not yet known that the parasite was host-specific. In 1976 the name Pneumocystis jiroveci was proposed for the first time, to distinguish the organism found in humans from variants of Pneumocystis in other animals. The organism was named thus in honor of Czech parasitologist Otto Jirovec, who described Pneumocystis pneumonia in humans in 1952. After DNA analysis showed significant differences in the human variant, the proposal was made again in 1999 and has come into common use.
The name was spelled according to the International Code of Zoological Nomenclature, since the organism was believed to be a protozoan. After it became clear that it was a fungus, the name was changed to Pneumocystis jirovecii, according to the International Code of Botanical Nomenclature (ICBN), which requires such names be spelled with double i (ii). Both spellings are commonly used, but according to the ICBN P. jiroveci has priority. A change in the ICBN in 2005 now recognizes the validity of the 1976 publication, making the 1999 proposal redundant, and cites Pneumocystis and P. jiroveci as examples of the change in ICBN Article 45, Ex 8. The name P. jiroveci is typified (both lectotypified and epitypified) by samples from human autopsies dating from the 1960s.
The term PCP, which was widely used by practitioners and patients, has been retained for convenience, with the rationale that it now stands for the more general Pneumocystis pneumonia rather than Pneumocystis carinii pneumonia.
The name P. carinii is incorrect for the human variant, but still describes the species found in rats and that name is typified by an isolate from rats.
Pneumocystis genome

Pneumocystis species cannot be grown in culture. Therefore, there is a limitation to the availability of the human disease causing agent, P. jiroveci. Hence, investigation of the whole genome of a Pneumocystis is largely based upon true P. carinii available from experimental rats which can be maintained with infections. Genetic material of other species, such as P. jiroveci can be compared to the genome of P. carinii.
The genome of P. jiroveci has been sequenced from a bronchoalveolar lavage sample. The genome is small, low in G+C content and lacks most amino acid biosynthesis enzymes.
History
.jpg/120px-Pneumocystis_jiroveci_-_Foamy_alveolar_cast_(5761923047).jpg)
The earliest report of this genus appears to have been that of Carlos Chagas in 1909 who discovered it in experimental animals but confused it with part of the life-cycle of Trypanosoma cruzi (causal agent of Chagas disease) and later called both organisms 'Schizotrypanum cruzi' a form of trypanosome infecting humans. The rediscovery of Pneumocystis cysts was reported by Antonio Carini in 1910 also in Brazil. The genus was again discovered in 1912 by Delanoë and Delanoë this time at the Pasteur Institute in Paris, France who found it in rats and who proposed the genus and species name Pneumocystis carinii after Carini.
Pneumocystis was redescribed as a human pathogen in 1942 by two Dutch investigators, van der Meer and Brug who found it in three new cases: a 3-month-old infant with congenital heart disease and in 2 of 104 autopsy cases - a 4-month-old infant and a 21-year-old adult. There being only one described species in the genus, they considered the human parasite to be P. carinii. Nine years later (1951) Dr. Josef Vanek at Charles University in Prague in Prague, Czechoslovakia showed in a study of lung sections from sixteen children that the organism labelled "P. carinii" was the causative agent of pneumonia in these children. The following year (1952) JÃrovec reported "P. carinii" as the cause of interstitial pneumonia in neonates. Following the realization that Pneumocystis from humans could not infect experimental animals such as rats, and that the rat form of Pneumocystis differed physiologically and had different antigenic properties, Frenkel was the first to recognize the human pathogen as a distinct species. He named it Pneumocystis jiroveci (see nomenclature above). There has been controversy over the relabeling of P. carinii in humans as P. jiroveci, which is why both names still appear in publications. However, only the name P. jiroveci is used exclusively for the human pathogen, whereas the name P. carinii has had a broader application to many species. Frenkel and those before him believed that all Pneumocystis were protozoans, but soon afterwards evidence began accumulating that Pneumocystis was a fungal genus. Recent studies show it to be an unusual, in some ways a primitive genus of Ascomycota, related to a group of yeasts. Every tested primate, including humans, appears to have its own type of Pneumocystis that is incapable of cross-infecting other host species and has co-evolved with each mammal species. Currently only 5 species have been formally named: P. jiroveci from humans, P. carinii as originally named from rats, P. murina from mice, P. wakefieldiae also from rats, and P. oryctolagi from rabbits.
Historical and even recent reports of P. carinii from humans are based upon older classifications (still used by many, or those still debating the recognition of distinct species in the genus Pneumocystis) which does not mean that the true P. carinii from rats actually infects humans. In an intermediate classification system, the various taxa in different mammals have been called formae speciales or forms. For example the human "form" was called Pneumocystis carinii f. [or f. sp.] hominis, while the original rat infecting form was called Pneumocystis carinii f. [or f. sp.] carinii. This terminology is still used by some researchers. The species of Pneumocystis originally seen by Chagas have not yet been named as distinct species. Many other undescribed species presumably exist and those that have been detected in many mammals are only known from molecular sample detection from lung tissue or fluids, rather than by direct physical observation. Currently, they are cryptic taxa.
References


